Vitamin D Deficiency and Covid-19:
Make D While the Sun Shines (And when the sun doesn’t shine, supplement)
Vitamin D deficiency is so widespread, and so predictive of bad health outcomes, that it has itself been called a pandemic by many scientists, even in the title of at least one peer-reviewed scientific paper1. Others have argued that widespread vitamin D deficiency may be a symptom, not a cause, of ill-health2. In A Hunter-Gatherer’s Guide to the 21st Century, Bret Weinstein and I contend that the rush to supplement with vitamin D is yet another example of reductionist, metric-heavy thinking that passes for modern medicine and science (excerpted here). Our broader point stands, including that we moderns are making matters worse with many of our lifestyle choices, such as spending too much time inside, and slathering ourselves with sunscreen when we do venture out. But with particular regard to whether WEIRD3os ought to supplement with vitamin D, we (both Bret and I) now believe that we were wrong.
Vitamin D is synthesized in your skin, upon exposure to the sun. It can also be acquired through the diet, although greater than 90% of the vitamin D supply of our species is understood to be derived from exposure to ultraviolet B light, specifically from the sun4. The farther you get from the equator, the less intense the sunlight is—and therefore the less capable it is of helping you create vitamin D. Winter, too, poses a problem for vitamin D synthesis, due both to the lower angle of the sun in the sky (such that its rays pass through more blocking atmosphere before reaching us), and the fewer hours that the sun is above the horizon. Compound the two—winter and high latitude—and nearly no vitamin D synthesis occurs. That said, vitamin D is stored in fat for a long time5, which is presumably part of how people who lived in far northern (or, far more rarely, far southern) climes survived the Winters without experiencing deficits, before vitamin D supplements existed. Also contributing to those people’s success was the consumption of vitamin D rich foods6, like fish, eggs, and organ meats, especially liver.
The majority of human tissues and cells have a vitamin D receptor. Vitamin D is understood to decrease the risk of chronic illnesses ranging from autoimmune disease to cardiovascular disease to infectious disease. Just a few specific health outcomes include that vitamin D deficiency causes bone and muscle weakness; and increasing vitamin D reduces the risk of fractures, falls, periodontal disease, and colorectal cancer7. Vitamin D deficiency is also associated with increased risk of metabolic syndrome8. Supplementation with vitamin D in infancy decreases the later development of type I diabetes9. Vitamin D deficiency is also a significant risk factor for HIV patients10, and likely increases susceptibility of populations to seasonal influenza11. This is consistent with growing evidence that vitamin D functions in regulating the immune system, has many anti-viral properties, and that supplementation with it provides protection against many respiratory infections12.
Given that the vast majority of our vitamin D is gained through sun exposure, it is also of interest to investigate what diseases and conditions correlate with sun exposure. Here are just two: Greater exposure to sunlight is associated with reduction of risk of developing multiple sclerosis13. Even more surprising, greater exposure to sunlight is also associated with a reduction in the risk of death from malignant melanoma14. Sunlight, it turns out, is good for you. Doctors and public health officials advising us all to restrict our sun exposure lest we get skin cancer were—once again—basing their recommendations on reductionist, a-evolutionary science, and likely caused more harm than good.
Should you be hungry for more details on the health implications of vitamin D deficiency, Holick 200715 provides an exhaustive review.
What are the risk factors for Vitamin D deficiency?
Because sunlight is our primary source of vitamin D, things that block or reduce sunlight are risk factors for vitamin D deficiency16:
Latitude: People who live at higher latitudes (closer to the poles, farther from the equator) are more likely to be vitamin D deficient than are those who live closer to the equator.
Season: Winter and early Spring at high latitudes: The Winter sun is too low in the sky, especially if you are far north (or south), to help with much, if any, vitamin D synthesis. It is also cold in the Winter, so the next two bullet points (indoor lifestyles and clothes) are even more common.
Indoor lifestyles: Walls, roofs, and even windows block the sun. People who spend most of their time indoors are more likely to be deficient.
Clothes and sunscreen, both of which cover your skin: If when you do go outside, you tend to cover yourself up, either with clothes or with sunscreen, you’re preventing your body from synthesizing vitamin D.
Skin color: People with darker skin are more likely to be vitamin D deficient than are people with lighter skin. Dark skin is endogenous sunscreen, an adaptation, broadly, to the tropical sun—darker skinned people are less likely to get sunburned, but also synthesize vitamin D at a slower rate than do lighter skinned people. As we have spread ourselves across the planet at an ever more rapid rate, however, far from where our ancestors lived when they first had the skin color that we have inherited, we run into some predictable problems. Light skinned people tend to burn fast near the equator. And dark-skinned people tend to be vitamin D deficient when living far from the equator.
There are also several diseases and conditions that may cause vitamin D deficiency, about which more below.
Is Vitamin D deficiency a risk factor for Covid?
In this era of abundant and prolific public health pronouncements and recommendations with regard to Covid, I have found none that advise the populace to check their vitamin D levels. (Please do share with me any that you find.)
What I do find are more than 11,000 results when I do a search on google scholar, limited to the years 2020 and 2021, for “Vitamin D deficiency and Covid.”17 Not all of those papers find evidence that there is a correlation, much less a causal relationship, between vitamin D deficiency and Covid. But it seems that most of them do. Nor have I assessed but a tiny minority of these papers. I read several reviews of the available literature, as well as haphazardly sampling papers, from both the “positive” (yes, there’s a relationship between vitamin D deficiency and poor Covid outcomes) and “negative” (no, there’s no relationship) categories. In my haphazard sample, the “positive” papers were largely well done, while the “negative” ones were either not all that negative, or obviously flawed.
So: Is vitamin D deficiency a risk factor for Covid? While I have already made clear that I find the evidence far more compelling and abundant for an affirmative answer to that question, let’s do two takes: No (negative), then Yes (positive).
Take one: Do not act! We don’t have enough data! For god’s sake do not take your health into your own hands!
I am only going to discuss two of the “negative” papers here: first Lordan 2021, an exhaustive review; then Rubin 2021, a very short review.
Lordan 2021
The title of this review paper18 explicitly suggests caution with respect to disagreement in the medical field about what molecular forms or indicators of vitamin D to measure, and how to classify and define vitamin D deficiency—which levels count as deficiency, for instance, and which as mere insufficiency. After describing all of the ways that the data aren’t clear, the paper allows that “Despite these confounding factors, the data would suggest that vitamin D deficiency does play a role in the incidence of COVID-19.”
Despite this, the author writes the following:
“Now that the coronavirus pandemic has reaffirmed its grip over the United States and Europe, the question is whether people should prophylactically increase vitamin D intake via diet and/or supplementation for future anticipated waves of infection? While it is always important to maintain a healthy and sufficient vitamin D status, the answer for COVID-19 prevention specifically is not straightforward.”
Before going on to acknowledge this:
“There is reasonable argument that it would be unwise not to supplement with vitamin D in high-risk groups, including the elderly, those with excess body fat, and the Black and minority ethnic groups, particularly African Americans who have a 6-fold higher COVID-19 mortality rate compared to white populations.”
However, the review continues, “most governments, medical organizations, and key leaders” are not recommending vitamin D supplements for the general population because of
“overstated claims for vitamin D in the past, the risk of overdose is possible (but unlikely), the evidence for a link to COVID-19 is still under consideration, and the public might over rely on the belief that taking vitamin D will make them ‘immune’ to COVID-19.”
To the question of overdose, this other review masterfully destroys such concerns, pointing out that industrial errors have been the cause of nearly all of the few cases known. As to the last point—that we must dissuade the public of the belief that this particular treatment will make them immune—I shouldn’t be surprised, at this point, to find arguments that are framed as if none of us can think for ourselves. The argument is basically: “We won’t provide any nuance in our recommendations, because we know that you, the populace, can’t handle it.” It is a lie of omission to keep us safe, or perhaps compliant, with what has been deemed “best” for us. It is worth noting that this requires no malice, only a belief that the narrative makers know best and an assumption that the population at large is not capable of making informed and logical choices.
I also recognize in this frame a mirror image: there is another treatment, one that is highly touted by public health officials, about which we are only allowed to discuss the positives, lest we recognize that complex systems are complex, and not all is as perfect as we have been led to believe (in, for instance, the land of Covid vaccines). Surely by now the officials in charge have begun to notice that artificially stark public health injunctions from on high leave a populace exhausted, angry, divided, and unhealthy.
In conclusion, Lordan allows this,
“While there is insufficient evidence to suggest that vitamin D is a viable therapeutic treatment for SARS-CoV-2 infection currently, those who may be deficient should increase their levels via diet, lifestyle, and supplementation as it is cheap and relatively safe to consume to attain any potential prophylactic benefits, but more importantly because maintaining an optimum vitamin D status is essential for general health.”
Rubin 2021
The other paper in the “negative” category that I want to mention is also a review, a short communication in the elite Journal of the American Medical Association (JAMA), which claims to be engaged in “Sorting Out Whether Vitamin D Deficiency Raises Covid-19 Risk19. It is, in short, exactly the kind of very brief read that doctors and other health care providers in clinical settings might rely on to inform their understanding of the science, which is why I’m choosing to mention it; it seems to have the potential to punch well above its weight. The article, which is less than two pages long, both reveals ignorance of some basics (such as how high latitudes and dark skin contribute differently to vitamin D deficiency), and misleads readers by focusing on bad science.
Rubin devotes a substantial portion of her review to a discussion of one paper (out of thousands of papers on the topic). The paper in question turned out to be fraudulent (so has been removed from pre-print servers). Scientific fraud is terrible. It skews our understanding of the world. But so does focusing on fraud (which is rare) rather than non-fraudulent evidence (which is abundant).
Motivated reasoning, low-quality work, and agenda-driven work are problems found in all arenas of science and public health. One fraudulent paper claimed to find a pattern, but its authors don’t even exist. Another paper claiming to review the literature focused tightly on said fraudulent paper, leaving the false impression that fraud is what you find when you go looking for evidence that vitamin D deficiency has a role to play in Covid outcomes. Alas, it seems that we might add to the list of pandemics that we are experiencing—Covid-19, vitamin D deficiency—motivated reasoning and incompetence, at least among our so-called experts.
Let’s try this again:
Is Vitamin D deficiency a risk factor for Covid?
Take two: It looks extremely likely, and that is really good news.
To start, let me remind the reader that even the “negative” papers tend to advise that, given how much other ill health and disease is understood to be the result of vitamin D deficiency, and given that so much of the WEIRD world in particular is understood to be deficient, supplementing with vitamin D can’t hurt, and it may well help.
There are a staggering number of studies that find a connection between vitamin D deficiency and poor outcomes from Covid. There are also some that fail to find a connection. The quality of the research varies; the study designs vary; the methods, sample sizes, countries, particular thing being measured—all of this varies between studies. And yet overwhelmingly, the pattern is clear.
Here, in a nutshell, is the upshot. It is a quotation from the abstract of an outstanding review20 published in September 2020 [author’s note, 10/27/21: this is a newer, even better review by the same author, Benskin, which demonstrates a causal relationship between vitamin D deficiency and poor Covid outcomes, and recommends target levels of vitamin D of 50ng/ml. I have not altered anything else in this text to reflect the newer review.]
“Although randomized controlled trial results may be available eventually, the correlational and causal study evidence supporting a link between vitamin D deficiency and COVID-19 risks is already so strong that it supports action…. Widely recommending 2,000 IU of vitamin D daily for all populations with limited ability to manufacture vitamin D from the sun has virtually no potential for harm and is reasonably likely to save many lives.”
Really, I could stop here. Readers who want to know more can do a “cited ref” search21 on the Benskin review. As of this writing, 70 other papers already cite her paper.
One of those 70 papers, itself a review22, concludes thusly:
“Given that vitamin D is a safe, inexpensive, and widely available agent, even in countries with limited resources, vitamin D inadequacy is obviously an easily modifiable risk factor. Therefore, from the literature reviewed here, prevention and/or restoration of vitamin D deficiency/insufficiency through vitamin D supplementation during the COVID‑ 19 period seems to be highly supported by the evidence.”
Among the many research papers that are not review articles, here are three that stood out to me.
An ecological study across 46 nations finds strong positive correlations between vitamin D deficiency and three Covid measures: incidence, complications, and mortality23. When vitamin D levels are low, bad Covid outcomes are high. This work looks at population-wide datasets, so while highly suggestive, does not provide evidence about individuals. Several observational studies are coincident with these conclusions, however, at the individual level, including:
185 patients who were retrospectively studied at a university hospital in Heidelberg, Germany24. These researchers found that “VitD deficiency was associated with a 6-fold higher hazard of severe course of disease and a ~15-fold higher risk of death.” This work was in fact, so compelling to some researchers that they responded with a short paper of their own, titled:
“Vitamin D insufficiency may account for almost nine of ten COVID-19 deaths: Time to act”25. Those responding begin their short piece this way:
“Evidence from observational studies is accumulating, suggesting that the majority of deaths due to SARS-CoV-2 infections are statistically attributable to vitamin D insufficiency and could potentially be prevented by vitamin D supplementation.”
Observation: Comorbidities for Covid-19 and conditions associated with vitamin D deficiency bear a striking resemblance.
Four of the most common conditions associated with vitamin D deficiency are also four of the most severe comorbidities for Covid-19: age, race, obesity, and kidney disease. (Using data from over half a million patients, over 13 months, this paper is an excellent source on the medical conditions that are Covid comorbidities)26.
Age: The older you are, the worse your likely outcome from Covid (this is one of the most widely known truths about Covid; here is one paper27 that discusses it). It is also true that as you age, you synthesize vitamin D less well, and are more likely to be vitamin D deficient28.
Race: African Americans (but not Africans) are at higher risk from Covid than are white Americans29. The darker your skin, the less efficient it is at synthesizing vitamin D, and so the more likely you are, especially if you also live far from the equator and spend most of your time inside, to be vitamin D deficient30.
Obesity: The higher your BMI, the worse your likely outcome from Covid; obese people are also more likely than non-obese people to be vitamin D deficient31.
Chronic kidney disease: is both a major comorbidity for Covid, and, as kidneys house the enzymes that are essential for the conversion of vitamin D into its circulating and hormonal forms, it should come as no surprise that vitamin D deficiency is also associated with chronic kidney disease32.
These aren’t all, either. While I find the following connections a bit less clear, it is also worth noting that the conditions that follow are comorbidities for Covid (or otherwise associated with either the risk of getting Covid, or bad outcomes if you do get it; again, this paper is my source on medical comorbidities for Covid), and also seem to be indicated in vitamin D deficiency:
Depression33 and anxiety disorders34, which when combined are in the top three medical comorbidities for Covid, have been linked to vitamin D deficiency.
Diabetes, both type I and type II: vitamin D deficiency is a contributing factor to the development of both types of diabetes (as briefly reviewed and empirically demonstrated here35), and is a Covid comorbidity.
Being institutionalized—as in a nursing or care home—is highly correlated with vitamin D deficiency, due to the lack of exposure to sunlight36. Many Covid deaths have been among the institutionalized.
The overlap between comorbidities for Covid and conditions associated with vitamin D deficiency raises an obvious question about the relationship: Is vitamin D deficiency causing these other conditions, and these conditions are (independent of vitamin D deficiency) comorbidities for Covid? Or is vitamin D deficiency causal in both Covid (infection and outcomes), and these other conditions? It seems like a very important question to answer.
There is considerable evidence that
there is a relationship between vitamin D deficiency and Covid;
many comorbidities for Covid are also demographic factors or conditions that are associated with vitamin D deficiency;
myriad other health conditions are associated with vitamin D deficiency;
there is widespread vitamin D deficiency among WEIRD populations in particular; and
vitamin D is not just safe but necessary.
Therefore, at this moment in time, everyone should be making sure that their vitamin D levels are sufficient. And the best way to do that, is by spending time in the sun.
How much sun exposure do you need?
At mid-Summer, many don’t need that much sun for their immediate needs, even if they’re fairly far from the equator. That is true, for those who are youngish, healthyish, and fair skinned. Change any of those parameters, and the amount of sunlight one needs in order to make sufficient amounts of vitamin D goes up, in some cases significantly.
In the United Kingdom, if one is a young, fair-skinned, healthy person, 2 – 3 days per week during the Summer, of 20 – 30 minutes of sunlight exposure midday, on the face and forearms, is sufficient to achieve healthy vitamin D levels37. That’s less than two hours per week of sun exposure over a fairly small part of your body. Remember, though, that age, skin color, BMI, and other health conditions all affect your ability to synthesize vitamin D. This also doesn’t take into account that winter is coming, and with it, far less sun. Better to bank a lot of vitamin D while the sun is high and bright in the sky.
In 1999, the British Journal of Medicine (BJM) published an article38 called “Are we really dying for a tan?”, which asked if people’s desire to get tan is, as we are often told, killing us. In an era before smart phones and social media, the authors observed that people do a kind of “lay epidemiology,” in which we interpret health risks by integrating information from multiple sources: personal observation; discussion of anecdotes of illness and death with friends and family; evidence, both formal and informal, that the media provide; and health education materials, some directly from health care professionals. In 1999, the authors claim, lay epidemiology held that exposure to sunlight was more beneficial than harmful. That is: most people weren’t buying the message that being in the sun was bad for you. The authors continue,
“This belief contrasts sharply with the current health education message. But before we dismiss this discordance between lay epidemiology and health education messages as ignorance on the part of the public, we should re-examine the scientific evidence on the overall balance of the benefits and harm of sun exposure.”
Indeed we should—and we should not only do so in this case, but anytime there is discordance between public health messaging and “lay epidemiology.” And we should remember, always, that it is the pinnacle of arrogance to assume that whatever it is that “the experts” believe now is in fact the truth, the whole truth, and nothing but the truth. Scientists have believed and public health officials have promoted many wrong things over the years, for both honorable, and not so honorable reasons. Sometimes the public health message is dead wrong.
Oh and by the way, even back in 1999, those authors of the BJM article concluded that the lay epidemiologists—that’s us, the public—were right. Being told to stay out of the sun, and slather ourselves with sunscreen every time we did go out—that was where the error was.
Vitamin D Supplements
All of that said, for many modern people, even regular exposure to sunlight is insufficient to keep their vitamin D levels up.
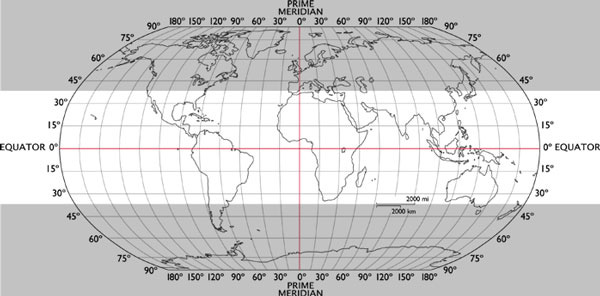
In the late Fall through early Spring, if you’re North of about the 35th parallel north (or South of the 35th parallel south), you won’t get enough exposure to ultraviolet B from the sun to make sufficient vitamin D. That’s roughly the grey zone on the world map below.
Consider this map: The 37th (rather than 35th) parallels are marked. In the southern hemisphere, only New Zealand and the tip of South America, including Buenos Aires, are in the grey zone. All of Australia is practically bathing in sunlight. In the northern hemisphere, however, practically all of Europe, a large fraction of mainland Asia, all of Canada, and a majority of the United States, are in the grey zone, in which supplementation with vitamin D during the dark months is likely to be important.
In 2013, Consumer Reports compared vitamin D supplements, and found that basically all of them are what they say they are. In supplements that include both vitamin D and calcium, however, Consumer Reports found that many contained lead, but are not legally required to state that on the bottles, for legal reasons that I did not pursue. But among the pure vitamin D supplements, there were no such issues, and buying based on price and your preferred form (e.g., tablet or gummy) seems fine. So, avoid the combined D + Calcium supplements, but in pure D3 supplement-land, everything seemed pretty rosy, at least as of 2013.
In conclusion
Go outside. Stand in the sun, and enjoy how it feels on your bare skin. Do not slather yourself with sunscreen before doing so, but if you are very fair or haven’t been in the sun for a while, know that your tolerance will be low. You don’t want to burn. Get in touch with how it feels to have your bare skin in the sun, and act accordingly.
And, depending on where you live and how you spend your time and who your ancestors were and how old you are and what underlying health conditions you have, consider supplementing with vitamin D. In fact, if you live North of the 35th parallel north (or South of the 35th parallel south), regardless of what else is true of you, you likely have a vitamin D deficiency, at least in the Winter and early Spring, and supplementing is a good idea.
If you have not already done so, begin to take your health back into your own hands. Listen to your body; move your body; feed it delicious, whole foods that your grandmother would recognize as food39; and—once again, today and always—go outside.
Subscribe for free and receive a post in your inbox every Tuesday. Paying subscribers are also able to comment on public posts, and receive both audio versions of the Tuesday posts, and occasional posts with links to other things that I’m thinking about these days.
Cashman et al 2016. Vitamin D deficiency in Europe: pandemic? The American journal of clinical nutrition, 103(4): 1033-1044.
Autier et al 2014. Vitamin D status and ill health: A systematic review. Lancet Diabetes & Endocrinology, 2(1): 76– 89.
Inhabitants of Western, Educated, Industrialized, Rich, Democratic countries
Pearce and Cheetham 2010. Diagnosis and management of vitamin D deficiency. BMJ, 340: 142-147.
Martinaityte et al 2017. Vitamin D stored in fat tissue during a 5-year intervention affects serum 25-hydroxyvitamin D levels the following year. The Journal of Clinical Endocrinology & Metabolism, 102(10): 3731-3738.
Lamberg-Allardt 2006. Vitamin D in foods and as supplements. Progress in biophysics and molecular biology, 92(1): 33-38.
Bischoff-Ferrari et al 2006. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. The American journal of clinical nutrition, 84(1): 18-28.
Chiu et al 2004. Hypovitaminosis D is associated with insulin resistance and β cell dysfunction. The American journal of clinical nutrition, 79(5): 820-825.
Hypponen et al 2001. Intake of vitamin D and risk of type 1 diabetes: a birth cohort study. Lancet 2001; 358:1500-3.
Akimbekov et al 2020. Effects of sunlight exposure and vitamin D supplementation on HIV patients. J Steroid Biochem. Mol. Biol.2020, 200: 105664.
Cannell et al 2006. Epidemic influenza and vitamin D. Epidemiol. Infect. 2006, 134: 1129–1140.
Beard et al 2011. Vitamin D and the anti-viral state. J. Clin. Virol. 2011, 50: 194–200.
Ponsonby et al 2002. Ultraviolet radiation and autoimmune disease: insights from epidemiological research. Toxicology, 181: 71-78.
Berwick et al 2005. Sun exposure and mortality from melanoma. Journal of the National Cancer Institute, 97(3): 195-199.
Holick 2007. Vitamin D deficiency. New England journal of medicine, 357(3): 266-281.
See Holick 2007, table 2, for a more thorough overview of causes of Vitamin D deficiency.
Since the original writing, but still before publication on October 26, 2021, that number has climbed to nearly 14,000 results, which seems improbable.
Lordan 2021. Notable developments for vitamin D amid the COVID-19 pandemic, but caution warranted overall: A narrative review. Nutrients, 13(3): 740.
Rubin, R., 2021. Sorting out whether vitamin D deficiency raises COVID-19 risk. JAMA, 325(4): 329-330.
Benskin 2020. A basic review of the preliminary evidence that COVID-19 risk and severity is increased in vitamin D deficiency. Frontiers in public health, 8: 513.
A “cited ref” search finds all of the papers that have cited that one you are looking at—it goes forward in time. To do a “cited ref” search, follow my link above, or: Find the paper in google scholar by pasting the title. Having found the paper, at the bottom of the reference, to the right of the quotation marks, click on “Cited by 70” (the number may have climbed by the time you get to it). Go to town: there are 70 more papers on this topic at your fingertips.
Sidiropoulou et al 2021. Unraveling the roles of vitamin D status and melanin during Covid‑19 (Review). International Journal of Molecular Medicine, 47(1): 92-100.
Mariani et al 2021. Association between vitamin D deficiency and COVID-19 incidence, complications, and mortality in 46 countries: an ecological study. Health security, 19(3): 302-308.
Radujkovic et al 2020. Vitamin D deficiency and outcome of COVID-19 patients. Nutrients, 12(9): 2757.
Brenner and Schöttker 2020. Vitamin D insufficiency may account for almost nine of ten COVID-19 deaths: Time to act. comment on: “Vitamin D deficiency and outcome of COVID-19 patients”. Nutrients 2020, 12, 2757. Nutrients, 12: 3642.
Kompaniyets et al 2021. Peer Reviewed: Underlying Medical Conditions and Severe Illness Among 540,667 Adults Hospitalized With COVID-19, March 2020–March 2021. Preventing Chronic Disease, 18: E66.
Davies et al 2020. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nature medicine, 26(8): 1205-1211.
Gallagher 2013. Vitamin D and aging. Endocrinology and Metabolism Clinics, 42(2): 319-332.
Golestaneh et al 2020. The association of race and COVID-19 mortality. E Clinical Medicine, 25: 100455.
Giménez et al 2021. Vitamin D deficiency in African Americans is associated with a high risk of severe disease and mortality by SARS-CoV-2. Journal of Human Hypertension, 35(4): 378-380.
Abbas 2017. Physiological functions of Vitamin D in adipose tissue. The Journal of steroid biochemistry and molecular biology, 165: 369-381.
González et al 2004. Vitamin D insufficiency and deficiency in chronic kidney disease. American journal of nephrology, 24(5): 503-510.
Anglin et al 2013. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. The British journal of psychiatry, 202(2): 100-107.
Casseb et al 2019. Potential role of vitamin D for the management of depression and anxiety. CNS drugs, 33(7): 619-637.
Parva et al 2018. Prevalence of vitamin D deficiency and associated risk factors in the US population (2011-2012). Cureus, 10(6).
Pearce and Cheetham 2010. (see footnote 4)
Ibid.
Ness et al 1999. Are we really dying for a tan? BMJ, 319(7202): 114-116.
Borrowed from Michael Pollan’s The Omnivore’s Dilemma.







Amazing the depth. Thank you, as always. I'm struggling with my explanation of why I have chosen to not be vaccinated. I don't have that "pitch" because I get distracted by, 'trumper', non-vaxxer, selfish, ... I believe none of those to be my personal reason yet I'm feeling pigeonholed even in my close group of friends and family. "Well, uh, I am 50ish, fit, eat well, exercise, get enough V-d, wear masks without any disgruntlement, wash my hands, social distance when needed...and uh, I'd rather wait and see what happens...? Because we don't have long term effects yet on these Vax's?" It accords with my understanding. Solo understanding, I guess, in my very polarized circles. Anyway, thanks for all yours and Bret's efforts to keep us all searching, reading and trying to be good humans.
Fact Check: TRUE